Glioblastoma multiforme is among the most lethal of cancers and the most stubborn in the face of treatment. Fewer than 20 percent of patients survive more than two years after diagnosis, according to the Central Brain Tumor Registry of the United States.
But a team of researchers at Fralin Biomedical Research Institute at VTC and City of Hope, a comprehensive care center, believes the complex way fluid flows through glioblastoma tumors holds the key to the therapy’s success. They believe they can use that flow to improve chimeric antigen receptor T cell therapy (CAR-T) and help more patients survive.
The National Institute of Neurological Disorders and Stroke, part of the National Institutes of Health, has awarded the team $3.75 million to study the impact of fluid flow on the therapy over the next five years.
“We believe we can actually encourage the T cells to move deeper into the tumor and search out those invading tumor cells in the brain and kill them,” said Jennifer Munson, associate professor at the Fralin Biomedical Research Institute.
Christine Brown, The Heritage Provider Network Professor in Immunotherapy, and Russell Rockne, director of the Division of Mathematical Oncology, both at City of Hope in Duarte, California, complete the multi-investigator team.
CAR-T cell therapy has been successful in treating a range of cancers. The method uses immune system cells called T cells that are genetically engineered to recognize and kill cancer cells. These engineered cells are injected into the patient’s body where they replicate and attack the tumor.
Brown has led the preclinical development and clinical translation of CAR-T cells for the treatment of glioblastoma at City of Hope and was part of the team that in 2017 successfully used CAR-T cell therapy to drive glioblastoma into remission in a patient.
But results of the therapy have been inconsistent from patient to patient, Munson said. The team’s study aims to identify the patient-specific factors that cause the therapy to work in some patients, but not others, while improving the therapy’s implementation.
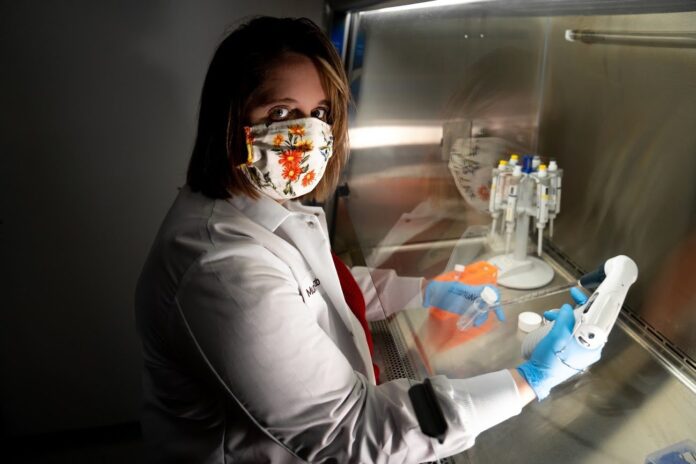
Munson’s lab at the Fralin Biomedical Research Institute will study the movement of liquid within human tissues, called interstitial fluid flow, to understand how beneficial T cells penetrate tumors. Munson specializes in engineering tissue models, so-called “tumors in a dish,” which can replicate the tumors of individual patients, so the researchers can see how the cells move inside a tumor.
Munson and Brown’s labs will work together to develop methods to adjust fluid flow to improve the effectiveness of the T-cell therapy. Ian Kimbrough, assistant professor in Virginia Tech’s College of Science, and John Rossmeisl, the Dr. and Mrs. Dorsey Taylor Mahin Professor at the Virginia-Maryland College of Veterinary Medicine, are part of the team for this aspect of the study.
“We want to know if we can deliver T cells into a specific part of the tumor, or at a specific flow rate or volume, to basically push the T cells around or move them where we need them to go,” said Munson, who also is an associate professor in the Department of Biomedical Engineering and Mechanics in Virginia Tech’s College of Engineering.
Rockne will build mathematical models to identify biomarkers to predict if the therapy will be effective in individual patients. He compared fluid flow through tumors to a river reaching the ocean, where it may leak in numerous directions.
“Glioblastomas disrupt the blood vessel network, creating leaky vessels, like river deltas, that create complicated flows within and around the tumor. Mathematics allows us to model and quantify how those complicated, river delta-like disrupted flows contribute to CAR-T cell migration and efficacy,” Rockne said.
Treatments and the survival rates for patients with gliobastomas haven’t improved in decades, Munson said. The team’s study affords an opportunity to contribute to progress in the ongoing enterprise of the research community to deploy multiple approaches to improve outcomes for patients with this disease.