Every 65 seconds, someone in the United States develops Alzheimer’s disease, a devastating form of dementia that affects 6.2 million Americans.
Though it was initially identified almost 120 years ago, Alzheimer’s disease is a progressive neurological disorder with no cure and few treatments. It starts out with minor memory loss that, over time, advances to a mental decline so severe, individuals have difficulty even swallowing.
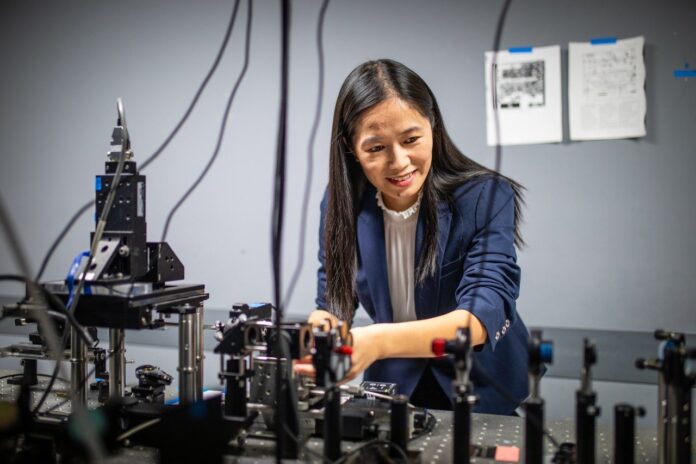
Xiaoting Jia, associate professor in the Bradley Department of Electrical and Computer Engineering, experienced the direct, cruel impact of Alzheimer’s disease as it ravaged her grandmother’s mind, destroying memories of a long-lived and loved life.
“Alzheimer’s is a devastating problem – I’ve seen firsthand how bad it could be,” Jia said. “It’s why it concerns me as an electrical engineer. I want to build tools and try to assist neuroscientists in solving brain problems.”
It’s this personal connection that makes the high priority, short-term grant from the National Institutes of Health so poignant.
Building a new fiber
A pioneer in the neural fiber field, Jia has partnered with longtime collaborator Harald Sontheimer, professor and chair of neuroscience at the University of Virginia, and fellow brain imaging expert Song Hu, associate professor of biomedical engineering at Washington University in St. Louis, on the development of a new neural tool: a deep brain, multipurpose fiber.
Their goal? Slowing down or reversing memory loss.
“What we are doing here together is creating a device with which we can visualize the build up of biomarkers that are the culprits of Alzheimer’s disease,” Sontheimer said. “Usually you can’t access or image that part of the brain, but this device will provide access to the hippocampus, home of spatial memory and retention.”
The team has one year to build a minimally invasive, long-term fiber – not much thicker than a strand of hair – to study those biomarkers, including thick protein deposits called amyloids in the hippocampus.
Current electrical and imaging tools by neuroscientists are limited in resolution, both time and spatial, such as an MRI or electroencephalogram. Some are more invasive with large electrodes with which doctors need to “fish” around in an attempt to apply electrical stimulation to the deep brain.
“A big problem in Alzheimer’s research is there are a lot of dysfunctions in the brain having to do with neurovascular changes,” Hu said, “but we don’t totally understand how those changes impact memory loss and behaviors that eventually impair their life. Conventional techniques have provided an important understanding of neurons and vasculature, but there’s a technology limitation.”
The super fiber Jia will construct stands out from other existing technologies because of the flexible polymer platform. Little to no damage of brain tissue and long-lasting potential means fewer complicated surgeries, and more time with family.
Defeating the deposits
“Amyloid deposits are the main feature for AD [Alzheimer’s disease], and they begin developing years, even decades, before people show AD symptoms,” Jia said. “It’s still a mystery how the deposits even begin.”
According to Jia, there’s no confirmed causal relationship between Alzheimer’s disease and the deposits – yet. However, the relationship between plaque buildup and the onset of symptoms is the guiding focus of the team’s research, with each researcher taking on a key component in the creation of this first-of-its-kind fiber:
- Building on expertise highlighted in her National Science Foundation Faculty Early Career Development (CAREER) award, Jia will thermally draw a multifunctional fiber for electrical stimulation and drug delivery, leaving a hollow core.
- In that core will go Hu’s dual-mode endoscope for capturing two different types of images in the brain.
- Sontheimer will develop the “chronic” implantation of the combined fiber and monitor the biocompatibility.

Target one for the team is to utilize the endoscope. It will provide images to the team for observing neuroactivity, the initial stages of amyloid deposition, and the blood flow in vessels. The team will use this data to analyze the memory loss-amyloid relationship.
Target two is sending electrical pulses – and later, anti-amyloid drugs – in the hopes of re-establishing blood flow and oxygenation to dead neurons and restoring memory.
If that sounds complex – it is. And the team only has 12 months to develop and test two prototypes.
“This is a very ambitious goal, what we’re trying to do in one year,” Jia said. “The brain is very nuanced with more than 80 billion neurons, and we’re still behind on fully understanding how the brain functions and how diseases are formed.”
Achieving its targets will enable the fiber team to seek additional multiyear funding from the National Institutes of Health. The ultimate hope? The researchers will be able to prove their technology has the possibility to improve the quality of life for the millions of Americans impacted by Alzheimer’s disease.
– Chelsea Seeber