Fatal overdose rates remain high in Virginia, even as the state begins to spread opioid settlement money to state and local agencies to help tackle the epidemic.
Death from drug overdoses, opioids and fentanyl in particular, has remained the dominant method of unnatural death in Virginia since 2013, according to the Virginia Department of Health. Overdoses ticked slightly down last year, but the number is forecast to remain about the same or higher this year.
The state’s opioid epidemic was officially declared a public health emergency in 2016, and opioid-related deaths increased 274% between 2012 and 2022, according to VDH data. The number of all fatal overdoses had a slightly lower spike in the same time period, at 228%.
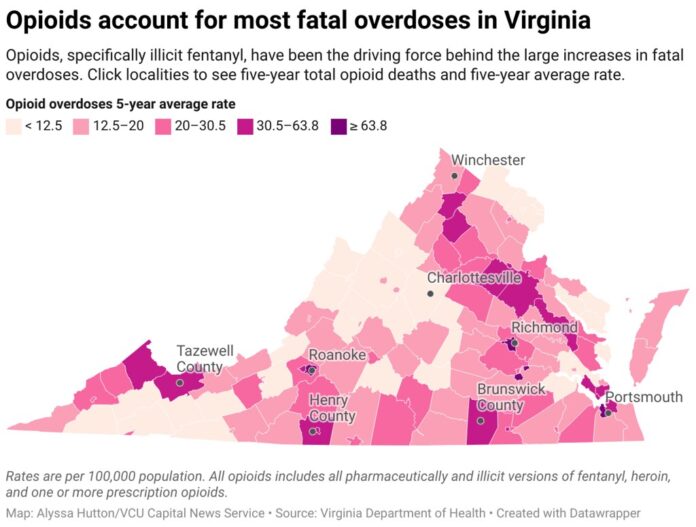
Overdose deaths from fentanyl had the biggest jump, increasing 3,866% in that same time. Richmond, Roanoke, Petersburg, Portsmouth and Hopewell cities had the highest rate of fatal opioid overdoses in 2022.
Virginia ranks 27th in the country for drug-related death rates and 15th for number of overall deaths, according to 2021 data from the Centers for Disease Control and Prevention.
‘It was a point of desperation’
Last year, Travis Williams realized that he felt miserable both on and off drugs. He lived mostly in isolation, going to work and coming home to use cocaine and heroin.
“It was a point of desperation where nothing was working no more,” Williams said. “Didn’t wanna go forward, didn’t wanna go back.”
He threw away all the drugs he had, including methadone, but said he didn’t experience withdrawal, which he credits to God. “I don’t want to kill myself, but I don’t want to live like this no more,” Williams said about the pivotal moment.
He has been sober for almost a year. He works with his best friend Jesse Wysocki, who he said he used to shoot heroin with, but now they’re both in recovery and helping others.
Wysocki is the chief operating officer at the McShin Foundation, a community recovery organization in Richmond with 16 recovery homes. The recovery program is 28 days long and available for anyone with substance use disorder, Wysocki said.
McShin does not offer detox or clinical services, although they help connect people with those programs.
McShin pairs people with a recovery coach. Wysocki, like most of the staff, are peer recovery specialists who have faced addiction. Peer recovery specialists are considered mentors and motivators to those struggling with addiction and go through a certification program by the Virginia Certification Board.
Wysocki says a recovery coach with experience helps in one’s personal recovery and also to support others.
“Whether I was in prison, jail, different treatment centers, so I know a lot of the behaviors that are associated with it,” Wysocki said. “So I’m able to help identify that, it helps me better assist who’s here trying to get services.”
For Williams, things came full circle when he was asked to work with McShin’s intensive program. That’s because of his first experience there in 2019. His then-recovery attempt ended with a relapse, and multiple doses of the medicine naloxone to reverse what could have been a fatal overdose — as it was for the friend he used with that night.
“I let my guard down and my disease started working with me,” Williams said. “If I just do a little bit, I’ll feel good.”
That fatal overdose triggered changes at McShin, Williams said. And he served a two and a half year stint in jail for violating his charges.
When Williams eventually returned to McShin, he agreed to work at the intensive housing program because he felt he had unfinished business.
“Just a little bit that I’ve learned, through that I can give it back … I find that like very fulfilling,” Williams said.
Williams is now a part of the McShin team that helps with the reentry transition from prison or jail.
3 in 4 overdoses from fentanyl
Fentanyl overdoses were over 75% of fatal overdoses in 2022 in Virginia.
This year’s number of fentanyl-related deaths is already over 1,000 and is expected to surpass last year’s number, according to VDH data. Cocaine and methamphetamine-related fatal overdoses have spiked in recent years in Virginia, due to being more commonly mixed with fentanyl.
Sgt. Kevin Wilson has been with the Virginia Beach Police Department for 18 years. He started with the narcotics unit of the special investigations department in 2010.
Wilson began to see the rise in opioid-use, specifically heroin, followed by the rise of fentanyl, not long after he started work with the narcotics unit.
“The majority of stuff we get contains part if not all fentanyl,” Wilson said.
Most illegal sellers and distributors aren’t chemists, so they’ll add a very potent substance such as fentanyl, Wilson said. That means a person’s normal dose could be more potent, which drives an increase in overdoses. People might not know what they are getting.
“The overall strategy would be to go after the highest level source of supply so we can cut the head off the snake,” Wilson said.
The industry is constantly evolving, he said, which presents challenges. “Once you take somebody off the street another person’s gonna take their place,” Wilson said.
Wilson has notified many families that they’ve lost a loved one to an overdose. “They want closure for themselves, for their loved one,” he said. “So being able to backtrack and go and find who sold them the drugs that caused them to to die and then bring closure for the families is probably the most satisfying.”
Virginia’s response to epidemic
Prescription opioid overdoses began to drop in 2015, with a significant recent decrease. Opioid manufacturers, wholesale distributors and pharmacies have been sued for their contributions to the opioid epidemic through overprescribing, deceptive marketing and dispensing.
The Virginia General Assembly established the Opioid Abatement Authority in 2021. The OAA provides funds for efforts that educate, treat and support recovery for people addicted to opioids, according to Anthony McDowell, executive director of the OAA.
Virginia’s estimated share of settlement money from the pharmaceutical industry is approximately $1.1 billion, as of September, according to a press release from state Attorney General Jason Miyares.
Grant applications for cities and counties began in January and the OAA approved over $23 million in June. This money is in the process of being transferred to its recipients, according to McDowell.
Localities requested OAA funding for a range of different tactics, according to McDowell.
“The cities and counties take stock of what the needs are at the community level and envision what it would take to address those needs and submit that in the form of a grant application to the OAA,” McDowell said.
The OAA also approved in August just under $11 million in funding for state agencies, including executive branch agencies, judicial offices and universities. Programs include clinical research, prevention and education, treatment, recovery and more. Approximately $2 million is earmarked for media and education campaigns.
The VDH will receive the highest allotment at $2.9 million for its four programs. The bulk of funding will go toward increasing access to naloxone, the generic form of Narcan, which can be used to reverse opioid overdoses. One million dollars will support harm reduction programs. The department will also hire three new “opioid specialists” for each health district.
The Virginia Department of Corrections will receive $1.25 million for programs such as hiring six social workers and creating an educational video. VADOC will also launch a pilot program to test the effectiveness of medicine used to treat moderate opioid use. The selected participants will use an injectable buprenorphine extended-release medication instead of suboxone.
Parental substance use is one of the reasons children are removed from their home. There was an increase of these cases from 2010-2019, according to the Virginia Department of Social Services. It’s common for family or friends to assume guardianship when a child is removed from the home. These guardians receive support through a kinship navigator program.
The DSS was given $205,500 to expand five kinship navigator programs, for the second half of 2024.
“As far as efforts that are being funded by the authority, it’s too soon to be able to take stock of the results yet,” McDowell said.
A locality’s use of settlement money depends on where the lawsuit originated, if they were a part of the lawsuit and whether the funds are being distributed directly from the settlement or from the OAA.
The OAA was recently nationally awarded for its settlement allocation efforts.
The state has made it easier since 2016 to procure naloxone over the counter without a prescription. The state also has a program to train people to recognize an opioid overdose and administer naloxone.
Patients cannot be prescribed more than a seven-day supply of controlled substances containing opioids, unless under certain conditions, due to a state law passed in 2017.
By Alyssa Hutton / Capital News Service